Authors:
R Leela*
II year B.E Biomedical Engineering, Agni College of Technology, Chennai, India
Received: 26 May, 2016; Accepted: 15 September, 2016; Published: 16 September, 2016
R Leela, II year B.E Biomedical Engineering, Agni College of Technology, Chennai, India, Tel: 7299257526; E-mail:
Leela R (2016) Biomaterial and Regenerative Medicine Approaches to Restoration of Flexion in Lumbar Herniated Disc. Glob J Biotechnol Biomater Sci 2(1): 019-024.
© 2016 Leela R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Objective: The systematic objective of this paper is to restore flexion in vertebral bone and to nourish the nucleus pulposus through the approach of biomaterial and regenerative medicine.
Method: Studies were made on the treatment of lumbar herniated disc in CINAHIL, PubMed, EMBASE, Cochrane Central Register of Controlled Trials (CENTRAL) and Cochrane Database of Systematic Reviews(CDSR). This paper provides methods for restoration of flexion in the bone. A biomaterial scaffold made of poly-β-hydroxybutyrate (PHB) consisting of extracellular matrix (ECM) proteins which is synthesized in vitro through regenerative medicine is replaced in the place of degenerated disc. The scaffold model is designed in CAD and then printed in LAB. The metabolic functions of the disc are performed by the scaffold.
Results: Fifteen papers, published between 2004 and 2014 were included in this study. Disc height restoration is possible using biomaterial and tissue engineering but none of the papers provide reports on flexion of the bone. The treatment of non-operative modalities like physical therapy, anti-inflammatory medications and steroid injections still results in low back pain. The surgical methods like Joint arthroplasty and non-fusion techniques spare motion but not restore normal spine biomechanics. The study shows that the treatment with cells and biomaterials shows better results.
Conclusion: Both the non-operative and surgical methods do not provide a good result. They do not offer flexion in the bone. The use of biomaterial scaffolds with ECM proteins paves a way for the medical professionals to treat lumbar herniated disc.
Introduction
Rationale
Degeneration of lumbar herniated disc is often associated with low back pain which affects up to 80% [1], of people. Acute pain recover within 10 weeks while chronic low back pain last for longtime. About 10% of people suffer from chronic low back pain [2]. In United States [3], the annual health care in case of chronic low back pain cost for 20 billion USD. The aging of the disc decreases [4,5], the cell density of the Nucleus Pulposus (NP) in the disc which in turn decline the production of extracellular matrix(ECM) proteins. The Nucleus Pulposus is covered by annulus fibrosus which is responsible to bear stress. The secretion of extracellular matrix contains proteins such as type 2 collagen [6] and aggrecans [7], which is the backbone of proteoglycan. There is also a pivotal role of the vertebral endplates in disc degeneration. The endplates are located in the cranial and caudal ends of each disc that separates the vertebral bone form the disc and prevents bulging of nucleus into adjacent vertebrae. The solute transport and maintenance is controlled by the proteoglycan molecules within the matrix. The blood vessels in the endplates are activated by degrading metalloproteinase (MMP) enzyme which are maintained in latent form by tissue inhibitors. The calcification of the vertebral endplate tremendously becomes less permeable for oxygen and nutrient supply [8], resulting in further degeneration of the disc [9]. The compressiblity of the disc is retarded due to the loss of hydrophilic proteoglycans within the NP cells. The recent treatments include the non-operative modalities such as physical therapy [10], anti-inflammatory medication [11] and steroid injection [12]. Surgical methods are used when there is a failure in the non-operative modalities. Surgical treatments include partial discectomy to spinal fusion [13,14], disc arthroplasty and non-fusion techniques spare motion and cannot restore normal spine biomechanics. So, there is no long term benefit [15]. Degeneration of disc is an important problem because the human beings face difficulty in their routine life.
Previous research [16-18], was focused on gene based delivery of growth factors into NP cells. Recent research focus on the combination of biomaterial and regenerative medicine based approach to degenerative disc disease to restore disc height. This approach helps in restoring disc anatomy and ECM production within the disc. Although disc height is possible to restore, the flexion in the disc is still a limitation. Hence the significance of this paper is restoration of flexion in the disc by using a special type of biomaterial along with the regenerative medicine as a scaffold which is replaced in the place of degenerated disc.
The NP cells [19,20] or bone marrow derived mesenchymal stem cells [21] are harvested and expanded in vitro and also coupled with poly-β-hydroxybutyrate which becomes a biomaterial scaffold and replaced in the place of degenerated disc.
Objective
The systematic objective of this paper is to restore flexion in the lumbar herniated disc through the combination of tissue engineering and biomaterial based approach. The primary end point is the restoration of the herniated disc to normal healthy disc and to improve tissue quality.
Materials and Methods
Composition of NP cells
The study deals with the method of replacing the herniated lumbar disc by combining biomaterial and regenerative medicine as a scaffold. The normal disc provides two major macro-molecular components in the extracellular matrix. The normal disc contains approximately 70% [22], proteoglycan and water content in the Nucleus Pulposus which is lesser in the Annulus fibrosis. The collagen network consist of type I and type II collagen fibrils which provides high tensile strength to the disc and anchors the tissue to the bone. Aggrecan is responsible for maintaining tissue hydration through osmotic pressure provided by its constituent chondroitin and Keratan Sulphate chains. Other collagen types are III, V, VI, IX, X, XI, XII, XIV, small proteoglycan such as lumican, biglycan, decorin and fibromodulin and other glycoproteins such as fibronectin and amyloid. The matrix is broken down by metalloproteinases(MMP) enzyme and aggrecans which also synthesize by disc cells. In degenerated disc type II collagen becomes denatured.
The level of decorin and biglycan is elevated in degenerated human disc. Fibronectin content increases with increasing degeneration and it becomes more fragmented. Therefore the level of proteoglycans is restored by stimulating the proliferation of NP cells by combining biomaterial and tissue engineering. The proteoglycans have an attraction to water and restores the normal biochemical environment and becomes rich in oxygen and nutrient supply. The combination of NP cells and poly-β-hydroxybutyrate as a scaffold is replaced in the place of degenerated disc by surgery. This helps in holding the vertebral bodies together. So, the disc becomes like a normal disc. Even in the case of injury the portion of scaffold is not injured and is very safe for human beings.
Poly-β-hydroxybutyrate
Poly-β-hydroxybutyrate is a polyhydroxyalkanoate a polymer belonging to polyesters class. PHB is probably the most common type of polyhydroxyalkanoate. PHB is produced by microorganisms such as Ralstonia eutrophus, Methylobacterium rhodesianum or Bacillus megaterium. The polymer is a product of carbon assimilation and is employed by microorganisms as a form of energy storage molecules to be metabolized when other common energy sources are not available. They have the property of resisting to biodegradation. They have good oxygen permeability therefore replacing it in the place of degenerated disc helps to nurture the cells with oxygen and nutrients. They have a melting point of 175 C and a glass transition temperature of 2 C which does not affect the body temperature of humans. Their tensile strength is 40 MPa close to that of polypropylene and so they are capable of bearing high tensile strength.By introducing the NP cells into poly-β-hydroxybutyrate and growing them in vitro and then replacing it in the place of degenerated disc the flexion in the disc is restored.
Cell based therapies
Main approach is to achieve cellular repair of the degenerated disc matrix. One approach is to stimulate disc cells to produce more matrix. It increases the rate of synthesis of matrix up to fivefold. Cytokines lead to loss of matrix because they inhibit matrix synthesis which stimulate agents that are induced in breakdown. The cell based therapies [23], are more advantageous than gene based therapies because it has to suite all persons.
Rapid prototyping technology
Products for making a biomaterial scaffold can be made through computer aided designing (CAD) in 3D and then it can be implemented in laser assisted bio-printing for printing the scaffold. The laser assisted bio-printing [24], setup is composed of a Nd:YAG laser, a microscopic objective and a ribbon positioned onto an XYZ translation stage. Each layer of the 3D image represents the shape of the cross-section of the model at a specific level. Rapid Prototyping technology is variously called solid free- form fabrication (SFF) or rapid manufacturing (RM). CAD enables computational modeling and finite element analysis (FEA) prior to fabrication. In this paper PHB biomaterial is scaffolded with NP cells and manufactured by rapid prototyping technology and then it can be implemented in the place of herniated disc.
Results
Study selection
Fifteen papers published between 2004 and 2014 are included in this study. The search produced 744 papers in total. It includes one hundred and forty three publications. Two foreign papers cannot be obtained.
Usually the investigation is made on few animals that develop disc degeneration spontaneously, such as the sand rat and chondrodystrophoid dog. Many biomaterials are related to help in recurring spinal problem. Among them poly-β-hydroxybutyrate plays a major role in providing the surface for attachment of extracellular matrix and proliferation of cells. The poly-β-hydroxybutyrate provides high tensile strength like the Annulus Fibrosis which would help in protecting Nucleus Pulposus consisting of the extracellular matrix proteins. Most of the papers deals with PLGA biomaterial which helps in delivering and proliferation but flexion along with stability is not there in PLGA. Disc height restoration is possible using PLGA but flexion is the bone is still a question. So, the remedy for that is Poly-β-hydroxybutyrate Table 1.
Figure 1 shows the schematic representation of the adult disc. It is a normal disc in a healthy human beings.
-
Figure 1:
Schematic representations of the adult intervertebral disc. (A) Mid-sagittal cross-section showing anatomical regions. (B) Three-dimensional view illustrating AF lamellar structure.
Figure 2 shows the MRI image of a degenerated disc [25] in which the NP cells are degenerating and the anterior part of the Annulus Fibrosis is shrinking.
-
Figure 2:
Magnetic resonance images illustrating different stages of human lumbar disc degeneration. (A) A healthy disc exhibiting distinct AF lamellae (AF) and central NP region (NP). (B) A disc exhibiting early stages of degeneration, including moderate height reduction, decreased NP signal intensity and inward bulging of AF lamellae (*). (C) A disc exhibiting advanced stages of degeneration, including severely reduced height, large fissure (*) and generalized structural deterioration. Images obtained using 7T Siemens scanner and a turbo spin echo sequence at 200 µm isotropic voxel resolution.
The NP cells are synthesized from mesenchymal stem cells or bone marrow cells in vitro. The environment is maintained. In this way the content of proteoglycan molecule is restored and the disc becomes like a normal disc. The table1 shows the different biomaterial used in different models and relatively the rate of health in humans is also shown. The results of other papers shows that introduction of genes inside the body has major drawbacks that affects the people immune system and can cause mutation in the body. The mutation of genes sometimes can cause cancer. Therefore the results shows that using tissue engineering is a best way to avoid those problems. The notochord is sterilized and grown in vitro and then it is introduced in the place of degenerated disc.
Figure 3 shows the stages of notochord transformation into the NP in the mouse embryo. This is provided in the paper on “Degeneration and regeneration of the intervertebral disc: lessons from development”, published on 2011.
-
Figure 3:
Stages of notochord transformation into the NP in the mouse embryo. Embryos were stained with Alcian Blue (Which marks glycosaminoglycans) and Picrosirius Red (Which marks collagen). At embryonic day (E) 12.5, the notochord (arrow) runs uninterrupted the length of the vertebral column. Sclerotome cells have condensed perichordially, and metameric patterning of future disc and vertebral body condensation is apparent. At E13.5, the notochord has begun to contract within the vertebral body regions and expand within the disc regions (arrow). At E14.5, the notochord has virtually disappeared from the vertebral bodies, persisting solely in the vertebral bodies. At postnatal age 1 month, vertebral bodies are fully ossified and the NP (arrow) contains a glycosaminoglycan-rich extracellular matrix surrounded by the collagenous AF. Scale bars: E12.5, E13.5 and E14.5: 200 µm (top) and 100 µm (bottom); neonate 400 µm (top) and 200 µm (bottom); 1 month 500 µm (top) and 400 µm (bottom).
Surgical treatments like partial discectomy to spinal fusion, disc arthroplasty and dynamic stabilization techniques results shows that they can spare motion but cannot restore normal spine biomechanics. Therefore the long term benefit is not there. The results of papers shows that the loss of hydrophilic proteoglycans within the NP disc is mainly responsible to reduce disc height and compressibility and the load distributing and shock absorbing capacity is also reduced.
The endplate [26], plays a major role in degeneration of disc because it is located in between the cranial and caudal ends of each disc that separates the vertebral bone from the disc. The endplate also holds the vertebral bodies together and helps in the maintenance and regulation of nutrients and water. Lumbar compression forces range from 800 N while standing upright and 3000 N during active lifting. The results shows that due to these forces the pressure is measured to vary from 0.4 MPa while lying to 1.5MPa while standing and sitting to 2.3MPa while lifting. By using poly-β-hydroxybutyrate which has a 40 MPa pressure to resist and therefore can be considered as the best biomaterial scaffold. This can even protect the endplates of the disc from getting degenerated. The activation of the enzyme metalloproteinase (MMP) is prevented so that the degeneration of the endplate is avoided.
Figure 4 shows the MRI image of degenerating endplate published in the paper “The role of vertebral endplate in low back pain” published in the year 2013.
-
Figure 4:
Midsagittal T1-weighted (A) and T2-weighted (B) magnetic resonance (MR) images of an L1-12 motion segment with poor end plate signal. (C) Corresponding ultra-short time-to-echo (UTE) MR image showing enhanced end plate signal. Arrows indicate end plate defects shown in fig.5A and 5B. (UTE imaging courtesy of Drs. Roland Krug and Misung Han, Department of Radiology, University of California, San Francisco).
The Table 2 shown in the below shows the physical properties of PHA in comparison with conventional plastics. This data is shown by the paper “Biosynthesis of polyhydroxyalkanoates” published in volume 6, number 3 in the year 2001.
-
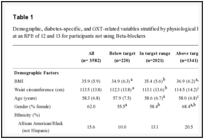
Table 2:
Physical properties of various PHA in comparison with conventional plastics.
From the table we can analyze that the PHB has a high tensile strength when compared to other polyhydroxyalkanoates. Although they have 5% elongation to break they can suite to the conditions of the human beings. PHB has a longer durability than PLGA bioploymer. So, results shows that the risk of getting injured is very small and can provide flexion in humans. It is evident from the paper published on disc height restoration that PLGA bioploymer can provide disc height but there is an unclear vision on flexion in the bone.
The results of papers also show that the female is more affected when compared to males and mostly in the lumbar region of the disc.
The Graph shows how many people are affected in the thoracic and lumbar region [27], according to their age group. The comparison is based on separation index.
The data from the graph is provided by the paper “Endplate changes related to age and vertebral segment” published in the year 2014 and volume 2014.
The Figure shown below is designed using computer aided designing for manufacturing the biomaterial scaffold in 2D. The designs are done for L3, L4 and L5 discs. The geometric dimensions of L3 disc is Upper vertebral width is 48.5±4.7 , lower vertebral width is 51.7±4.8, upper vertebral depth is 34.6±3.6, lower vertebral depth is 35.3±3.6 and disc height is 11.6±1.8. For L4 disc the upper vertebral width is 52.2±5.1, lower vertebral width is 52.5±4.7, upper vertebral depth is 35.7±3.7, lower vertebral depth is 36.2±3.7 and disc height is 11.3±2.1. For L5 disc the upper vertebral width is 52.2±5.1, lower vertebral width is 53.1±6.0, upper vertebral depth is 35.7±3.7, lower vertebral depth is 36.0±4.0 and disc height is 10.7±2.1. All these models are designed for both males and females in a survey made with 126 patients (Figure 5-7).
-
Figure 5:
Comparison of the separation index (SI) in the thoracic (T7-T8) and lumber (L4-L5) groups. Specimens from cadavers ≤40 years old and ≥40 years old were compared. Errors bar indicate the standard deviation.
-
Figure 6:
Comparison of the separation index (SI) in the ≤40 years and ≥40 year’s groups. Thoracic and lumbar segments were compared. Errors bars indicate the standard deviation.
-
Figure 7:
Comparison of the separation extension index (SEI) in the ≤40 years, ≥40 years, lumbar and thoracic groups. *Groups with statistical difference.
Discussion
Summary of evidence
The degeneration of the disc in the lumbar region is a major problem because it is a major difficulty in the human life. The composition of Nucleus Pulposus is altered during degenerated condition and there is a change in the physical and chemical structure of the disc. Due to this the Annulus Fibrosis gets shrinked and there is loss of type II collagen in the disc which in turn produces a loss in proteoglycan molecules. The proteoglycan molecule have the tendency to attract water and is capable of nourishing the NP cells. To protect the disc from herniation there is a new approach which can restore flexion in the bone and prevents it from getting degenerated. The approach shown in this paper is using a special type of biomaterial known as poly-β-hydroxybutyrate which provides a surface for attachment of extracellular matrix proteins synthesized by NP cells. The poly-β-hydroxybutyrate can withstand a tension of 40 MPa and is capable of bearing load. It has a melting point of 175 C and a glass transition temperature of 2C.So, there it doesn’t affect other body parts. It is also permeable to oxygen and nourishes the NP cells. In this process the composition of Nucleus Pulposus is restored. The type II collagen is restored and provides a high tensile strength to the bone. This method is considered the best way because in gene transfer the method of transferring the gene can affect the people and have the chances of getting mutated. If the genes are mutated then it can have the chance of getting cancer in people. The method provided in this paper is the easiest way because the NP cells are synthesized in vitro and can combine with a biomaterial made of biopolymer and through surgery the scaffold is replaced in the place of degenerated disc. This method can be tested using sand rat and chondrodystrophoid dog because these animals develop disc degeneration spontaneously. The animal to be considered for this method should mainly consist of type II collagen so that it would be evident to introduce this method in humans. This scaffold can prevent the vertebral endplates from getting degenerated. The tissue engineering does not have any limitations when compared to gene transfer method. The gene transfer method has a much higher cost when compared to tissue engineering. The results of the graph shows that women is more affected than men and that too mainly it affects the lumbar region of the disc.
-
Graph 8:
Limitations
Like other systematic reviews the validity of findings is affected by the availability and quality of primary data. The study in the Journal of Bone and Joint Surgery published between 1984 and 1999 pooled a mean of 43 studies. This paper deals only about the methods that can be possible to be introduced in humans with the analysis of data given in other papers but does not have any practical results paving the way for the future researchers to investigate on this and provide a better result for the patients with degenerated disc disease. The method of tissue engineering [28], is done with more cost and is not affordable by average peoples. The animals used for testing should mainly have type II collagen with them although they have type I collagen. This is one of the characteristic property which helps to transfer it to humans without any obstacle.
Conclusion
The combination of biomaterial with tissue engineering is considered the best way because it does not affect the human beings. The usage of poly-β-hydroxybutyrate can help the people with degenerated disc disease to restore to normal disc which can further help in the motion and therefore provides flexion in humans. Injection of NP cells does not provide a good way to cure when compared to surgery because it might have the chance of deviating from the herniated place.
The data is obtained from different authorized papers and is analyzed in this paper. This paper paves way for the future research to be done based on this idea.
-
-
- Rubin DI (2007) Epidemiology and risk factors for spine pain. Neurol Clin 25: 353-371.
- Kovacs FM Abraira V, Zamora J, Fernandez C (2005) The transition from acute to subacute and chronic low back pain: a study based on determinants of quality of life and prediction of chronic disability. Spine (Phila Pa 1976) 30:1786-1792.
- Katz JN (2006) Lumbar disc disorders and low back pain: socioeconomic factors and consequences. J Bone Jt Surg Am 88: 21-24.
- Antoniou J, Steffen T, Nelson F, Winter bottom N, Hollander AP, et al. (1996) The human lumbar intervertebral disc: evidence for changes in the biosynthesis and denaturation of the extracellular matrix with growth, maturation, ageing and degeneration. J Clin Invest 98: 996-1003.
- Buckwalter JA (1995) Aging and degeneration of the human intervertebral disc. Spine (Phila Pa 1976) 20: 1307-1314.
- Antoniou J, Goudsouzian NM, Heathfield TF, Winterbottom N, Steffen T, et al. (1976) The human lumbar endplate. Evidence of changes in biosynthesis and denaturation of the extracellular matrix with growth, maturation, aging and degeneration. Spine (Phila Pa 1976) 21: 1153-1161.
- Mwale F, Roughley P, Antoniou J (2004) Distinction between the extracellular matrix of the nucleus pulposus and hyaline cartilage: a requisite for tissue engineering of intervertebral disc. Eur cell Mater 8: 58-63.
- Rajasekaran S, Babu JN, Arun R, Armstrong BR, Shetty AP, et al. (1976) ISSLS prize winner: a study of diffusion in human lumbar discs: a serial magnetic resonance imaging study documenting the influence of the endplate on diffusion in normal and degenerate discs. Spine (Phila Pa in 1976) 29: 2654-2667.
- Urban JP, Smith S, Fairbank JC (2004) Nutrition of the intervertebral disc. Spine (Phila Pa 1976) 29: 2700-2709.
- Van Tulder MW, Malmivaara A, Esmail R, Koes BW (2000) Exercise therapy for low back pain. Cochrane Database Syst Rev 2000: CD000335.
- Cherkin DC, Wheeler KJ, Barlow W, Deyo RA (1998) Medication use for low back pain in primary care. Spine (Phila Pa1976) 23: 607-614.
- Buttermann GR (2004) The effect of spinal steroid injections for degenerative disc disease. Spine J 4: 495-505.
- Mariconda M, Galasso O, Attingenti P, Federico G, Milano C (2010) Frequency and clinical meaning of long term degenerative changes 0after lumbar discectomy visualized on imaging tests. Eur Spine J 19: 136-143.
- Kumar MN, Jacquot F, Hall H (2001) Long-term follow up of functional outcomes and radiographic changes at adjacent levels following lumbar spine fusion for degenerative disc disease. Eur Spine J 10: 309-313.
- Botelha RV, Moraes OJ, Fernandes GA, Buscariolli YS, Bernardo WM (2010) A systematic review of randomized trials on the effect of cervical disc arthroplasty on reducing adjacent level degeneration. Neurosurg Focus 28: E5.
- An HS, Takegami K. Kamada H, Nguyen CM, Thonar EJ, et al. (2005) Intradiscal administration of osteogenic protein-1 increases intervertebral disc height and proteoglycan content in the nucleus pulposus in normal adolescent rabbits. Spine (Phila Pa 1976) 30: 25-31.
- Imai Y, Okuma M, An HS, Nakagawa K, Yamada M, et al. (2007) Restoration of disc height loss by recombinant human osteogenic protein-1injection into intervertebral discs undergoing degeneration induced by an intradiscal injection of chondroitinase ABC. Spine (Phila Pa 1976) 32: 1197-1205.
- Masuda K, Imai Y, Okuma M, Muehleman C, Nakagawa K, et al. (1976) Osteogenic protein-1 injection into a degenerated disc induces the restoration of disc height and structural changes in the rabbit anular puncture model. Spine (Phila Pa 1976) 31: 742-754.
- Nishunura K, Mochida J (1998) Percutaneous reinsertion of the nucleus pulposus. An experimental study. Spine (Phila Pa 1976) 23: 1531-1538.
- Okuma M, Mochida J, Nishimura K, Sakabe K, Seiki K (2000) Reinsertion of stimulated nucleus pulposus cells retards intervertebral disc degeneration: an in vitro and in vivo experimental study.[Orthop Res 18: 988-997.
- Sakai D, Mochida J, Iwashina T, Hiyama A, Omi H, et al. (2006) Regenerative effects of transplanting mesenchymal stem cells embedded in atelocollagen to the degenerated intervertebral disc. Biomaterials 27: 335-345.
- Yong-Soo Choi (2009) Pathophysiology of degenerative disc disease. Asian Spine J 3: 39–44.
- Oehme D, Goldschlager T, Ghosh P, Rosenfeld JV, Jenkin G (2015) Cell based therapies used to treat 5lumbar degenerative disc disease: A systematic review of animal studies and human clinical trials 2015. ID 946031.
- Devillard R, Pagès E, Correa MM, Kériquel V, Rémy M, et al. (2014) Muhammad Ali Cell patterning by laser-assisted bioprinting. Methods Cell Biol 119: 159-174.
- Smith LJ, Nerurkar NL, Choi KS, Harfe BD, Elliott DM (2011) Degeneration and regeneration of the intervertebral disc: lessons from development. Dis Model Mech 4: 31-41.
-
-
-
-
-



 Global Journal of Biotechnology and Biomaterial Science
Global Journal of Biotechnology and Biomaterial Science




Table 1:
Provided in the paper for Disc height restoration published in the year 2012.